Background on the DRA
The federal Deficit Reduction Act of 2005 (DRA) included new requirements related to fraud, waste and abuse for Medicaid plans that received or made payments of $5 million dollars or more in any fiscal year. Section 6032 of the DRA requires all subject entities to establish written policies that provide detailed information about:
- the Federal False Claims Act
- the administrative remedies for false claims and statements
- applicable state laws that provide civil or criminal penalties for making false claims and statements
- the “whistleblower” protections afforded under such laws
- the role of such laws in preventing and detecting fraud, waste and abuse in federal health care programs.
Entities are required to create and disseminate these written policies, either on paper or electronically, to all employees as well as their contractors and agents. In turn, it is the responsibility of each contractor and agent to adopt these policies, which must be readily available.
States have created various reporting mechanisms for their Medicaid contractors to report compliance with the provisions of the DRA. Many states opted to create state laws regarding false claims and whistleblower protections so compliance reporting will include not only the federal requirements but also state mandates. States may choose to confirm Medicaid contractor compliance through a variety of mechanisms.
Compliance Certification in New Jersey
In a September 2016 Newsletter (Volume 26, No. 14) published jointly by a number of New Jersey state agencies, the state Comptroller’s Medicaid Fraud Division set forth the action required of Medicaid Managed Care Organizations (MCOs) related to the identification and exclusion of individuals from federal programs. The newsletter provided a list of databases that must be screened monthly to verify that any current or prospective employees, contractors or subcontractors who directly or indirectly serve Medicaid programs are not excluded or otherwise prohibited from participation.
In New Jersey, contractors are required to annually submit a “Certification of Compliance” with Section 6032 of the Federal Deficit Reduction Act of 2005 (the “form”), which is the section pertaining to prevention and detection of fraud, waste and abuse in federal healthcare programs. As noted on the form, any provider that received or made payments of $5 million or more (in the aggregate) of federal Medicaid funds during the previous federal fiscal year is required to submit certification of compliance. A provider’s contractors, as defined, are also required to comply with the Section 6032 fraud, waste and abuse policy and education requirements. Section C of this form addresses the monthly background checks required to identify excluded individuals or entities, to ensure that no federal funds are paid to such providers.
On January 11, 2022 the New Jersey Comptroller’s Office Medicaid Fraud Division issued a notice to subject providers regarding a newly updated Certification of Compliance form to be used starting in 2022. Subject entities were required to submit the completed form for the previous federal fiscal year (October 1, 2020 – September 30, 2021) within 30 days of the notice issuance date. The state Medicaid Fraud Division also provided a summary of document submission requirements to substantiate compliance with Section 6032.
It was recently noted that the updated 2022 certification form and the 2016 Newsletter may differ on which databases must be screened to meet compliance. It appears that screening the N.J. Department of Health licensure database is no longer mandatory. This apparent discrepancy has been raised with the Comptroller’s Office but to date, no response has been provided. N.J. Medicaid contractors, subject to the DRA requirements, who have concerns should refer the question to their legal counsel or reach out to the New Jersey Medicaid Fraud Division for a definitive interpretation.
The 2016 Newsletter lists seven screening databases that are listed as either mandatory or mandatory if applicable. The 2022 DRA Certification of Compliance (the “form”) lists six screening databases. The area of discrepancy relates to item 5 on the 2022 form and items 5 on the Newsletter.
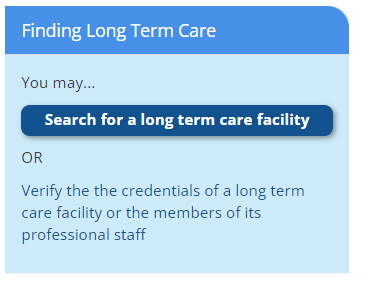
- The 2016 Newsletter, Item 5, lists the NJ Department of Health licensure database as a mandatory list to check and provides a link to the Department of Health Facilities page (http://www.state.nj.us/health/guide/find-select-provider).
- The 2022 form does not include a link to the N.J. Department of Health licensure database nor list it as a mandatory list to screen against.
On that Facilities page, in the lower right-hand corner, is a link to the database of N.J. licensed/ certified staff of long-term care and assisted living facilities. There appears to be no other database referenced on that page that could be screened.
Also, a Google search of “N.J. Depart of Health licensure database” (which is the title of item 5 on the 2016 Newsletter), directs users to http: Department of Health | Health Facilities | Licensing and Certification Credentials (nj.gov) which addresses certification and licensing of long-term care and assisted living staff and provides a link to a searchable database in the lower left-hand corner.
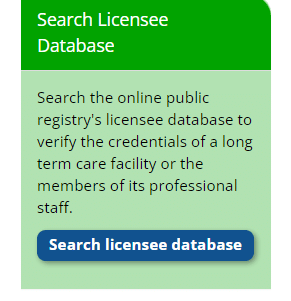
Using this “Search licensee database” link, users are directed to the same page to which the url listed in Section 1-c(v) of the 2022 Certification of Compliance form (https://njna.psiexams.com/search.jsp) directs users:
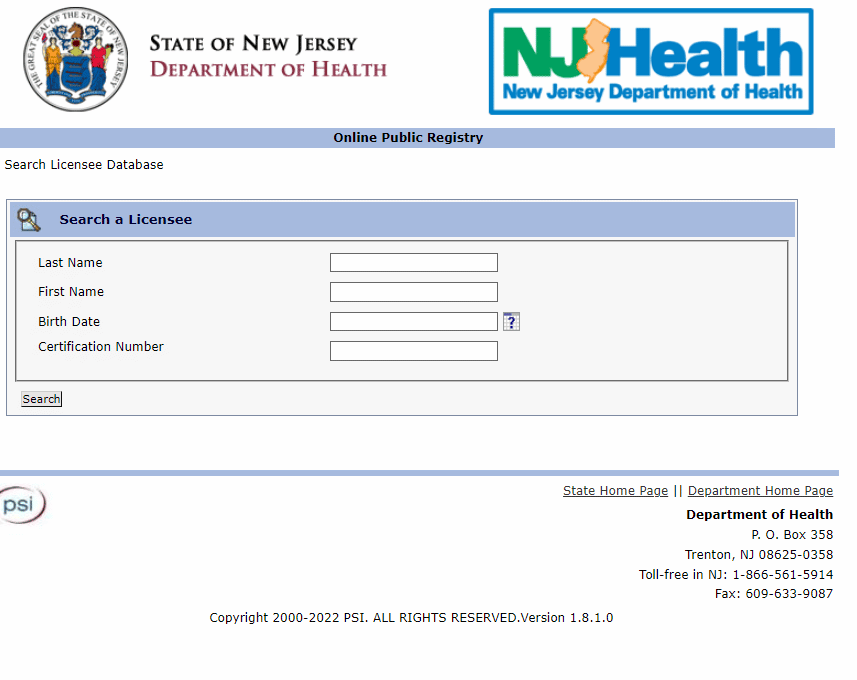
Therefore, it appears that the change to the 2022 form Section 1-c(v), which eliminated the link to the Department of Health | Your Guide to Health in New Jersey (state.nj.us) on item 5 of the 2016 Newsletter, was made because the License Management link directs users to the same place.
Conclusion
If a New Jersey Medicaid contractor has questions about whether there is some other database being referenced on item 5 of the 2016 Newsletter, seeking legal or regulator guidance to assure that they are meeting state requirements is highly recommended. Hopefully the state will issue clarification at some point so that contractors are provided with definitive direction on expectations. Streamline Verify screens against all federally and state-required lists as they apply to our clients’ organizations and needs.

































