History and Authority of Medicaid Fraud, Waste & Abuse Enforcement
The New York Department of Health includes the State Medicaid Agency as well as the Office of Medicaid Inspector General (OMIG). Among other functions, OMIG serves as the program integrity unit for the State’s Medicaid program.
The Office of the Medicaid Inspector General (OMIG) is an independent entity within the New York State Department of Health to promote and protect the integrity of the Medicaid program in New York State. The Medicaid Inspector General reports directly to the Governor.
In 2006, the state legislature amended the New York State (NYS) Executive, Public Health, Social Services, Insurance, and Penal laws to create OMIG and institute the reforms needed to effectively fight fraud and abuse in the State’s Medicaid program. The statutory changes separated the administrative and program integrity functions, while still preserving the single state agency structure required by federal law.
OMIG is charged with coordinating the fight against fraud and abuse in the Medicaid program. In carrying out its mission, OMIG conducts and coordinates the investigation, detection, audit, and review of Medicaid providers and recipients to ensure they are complying with the laws and regulations. To fulfill its mission, OMIG performs audits, investigations, and reviews of Medicaid services and providers and works closely with the federal Centers for Medicare and Medicaid Services (CMS), the Office of the Inspector General (OIG), the New York State Attorney General’s Medicaid Fraud Control Unit (MFCU), the Bureau of Narcotic Enforcement (BNE), and law enforcement and other state agencies. OMIG has the authority to pursue civil and administrative enforcement actions against any individual or entity that engages in fraud, abuse, illegal or inappropriate acts, or unacceptable practices. Information and evidence relating to suspected criminal acts are referred to the Attorney General.
Mission Statement
The mission of OMIG is to enhance the integrity of the NYS Medicaid program by preventing and detecting fraudulent, abusive, and wasteful practices within the Medicaid program and recovering improperly expended Medicaid funds, while promoting high quality patient care.
Exclusion and Screening – Regulatory Authorities in New York
The OMIG List of Restricted and Excluded Providers, which is the state’s Medicaid exclusion list, identifies individuals or entities who have been excluded from participating in the NY State Medicaid program under the provisions of 18 NYCRR § 515.3 and/or 18 NYCRR § 515.7. OMIG is responsible for managing provider exclusions and reinstatements.
188 NYCRR 515.3: Authority to sanction.
- Upon a determination that a person has engaged in an unacceptable practice , the department may impose one or more of the following sanctions:
- exclusion from the program for a reasonable time;
- censure; or
- conditional or limited participation, such as requiring preaudit or prior authorization of claims for all medical care, services or supplies, prior authorization of specific medical care, services or supplies, or other similar conditions or limitations.
- The department may also require the repayment of overpayments determined to have been made as a result of an unacceptable practice.
- Whenever the department sanctions a person, it may also sanction any affiliate of that person; provided, however, that in imposing a sanction upon an affiliate, the determination must be made on a case-by-case basis giving due regard to all the relevant facts and circumstances leading to the original sanction.
- In determining whether or not to sanction a person, the department may hold that person responsible for the conduct of another person. However, conduct may only be imputed to another when the persons are affiliates of each other, and the conduct was accomplished within the course of the duties of the person to be sanctioned and the other person knew or should have known of the conduct, or the conduct was effected with the knowledge and consent of the other.
18 NYCRR 515.7 Immediate sanctions.
- Notwithstanding any provision of this Title to the contrary, the department, upon notice to the person, may take immediate action under this section.
- Upon receiving notice of an indictment which charges a person with committing an act which would be a felony under the laws of New York and which relates to or results from:
- the furnishing or billing for medical care, services or supplies; or
- participation in the performance of management or administrative services relating to furnishing medical care, services or supplies, the department may immediately exclude the person and any affiliates, and may continue the exclusion for 90 days following receipt of notice of the disposition of the indictment.
- Upon receiving notice that a person has been convicted of a crime which relates to or results from:
- the furnishing of or billing for medical care, services or supplies; or
- participation in the performance of management or administrative services relating to furnishing medical care, services or supplies, the department may immediately exclude the person and any affiliates from participation in the program.
- Upon determining that the public health or welfare or the health or welfare of a recipient would be imminently endangered by the continued participation of any person in the program, the department may immediately exclude the person and any affiliates until the conditions giving rise to the exclusion have been corrected or a further investigation determines that there is insufficient evidence to support a continued exclusion.
- Upon receiving notice that a person has been found to have violated a State or Federal statute or regulation pursuant to a final decision or determination of an agency having the power to conduct the proceeding and after an adjudicatory proceeding has been conducted, in which no appeal is pending, or after resolution of the proceeding by stipulation or agreement, and where the violation resulting in the final decision or determination would constitute an act described as professional misconduct or unprofessional conduct by the rules or regulations of the State Commissioner of Education or the State Board of Regents, or an unacceptable practice under this Part, or a violation of article 33 of the Public Health Law, the department may immediately sanction the person and any affiliate.
- Where the department is authorized to exclude a person under this section, it may impose a less severe sanction, if a lesser sanction would be in the best interest of the program.
- Appeals.
- A person sanctioned under this section is not entitled to an administrative hearing, but may, within 30 days of the date of the notice, submit written arguments and documentation on the following issues:
- whether the determination was based upon a mistake of fact;
- whether any crime charged in an indictment, or any conviction of a crime, resulted from furnishing or billing for medical care, services or supplies; and
- whether the sanction imposed was reasonable.
- Within 45 days of receiving written arguments or documentation in response to an immediate sanction, the department will review the determination and notify the person sanctioned of the results of that review. After the review, the determination to immediately sanction the person may be affirmed, reversed or modified, in whole or in part.
- A person sanctioned under this section is not entitled to an administrative hearing, but may, within 30 days of the date of the notice, submit written arguments and documentation on the following issues:
Effect of Exclusion
The effect of exclusion is wide ranging, as noted in 18 NYCRR 515.5:
- No payments will be made to or on behalf of any person for the medical care, services or supplies furnished by or under the supervision of the person during a period of exclusion or in violation of any condition of participation in the program. In the case of a hospital, nursing home or home health care provider, the department may continue payments for up to 30 days after the date of exclusion for clients admitted prior to the exclusion or whose plan of care was implemented prior to the exclusion.
- No payment will be made for medical care, services or supplies ordered or prescribed by any person while that person is excluded, nor for any medical care, services or supplies ordered or prescribed in violation of any condition of participation in the program. The department may pay the first claim(s) submitted by or on behalf of a dispensing provider for care, services or supplies ordered or prescribed by an excluded person after the date of exclusion and notify the dispensing provider of the exclusion. The department may not pay for any care, services or supplies ordered or prescribed by an excluded person more than 20 days after the date of a notice of an exclusion to a dispensing provider.
- A person who is excluded from the program cannot be involved in any activity relating to furnishing medical care, services or supplies to recipients of medical assistance for which claims are submitted to the program, or relating to claiming or receiving payment for medical care, services or supplies during the period.
- Providers reimbursed on a cost-related basis may not claim as allowable costs any amounts paid or credited to any person who is excluded from the program or who is in violation of any condition of participation in the program.
- Providers reimbursed on a fee-for-services basis may not submit any claim and cannot be reimbursed for any medical care, services or supplies furnished by any person who is excluded from the program or which are furnished in violation of any condition of participation in the program.
No Right to Appeal an Immediate Sanction
It should be noted that there is no right to appeal an immediate sanction but parties can submit written arguments and documentation regarding whether the determination was based upon a mistake of fact, whether any crime charged in an indictment, or any conviction of a crime, resulted from furnishing or billing for medical care, services or supplies; and whether the sanction imposed was reasonable. (18 NRCRR 515.7(g)).
Requests for Reinstatement
If excluded, a party must submit an application for reinstatement if the party wishes to be enrolled/reinstated into the Medicaid program. OMIG has 90 days to complete its review and render a decision. (This timeframe may be extended if OMIG or the New York State Department of Health (DOH) requires more time to review the application and sends a letter for extension to the applicant, or if OMIG or DOH sends a letter requesting information to the applicant.) Decisions are based on information submitted with the application or letter. If the applicant is denied enrollment or reinstatement based upon prior conduct, the applicant cannot re-apply for enrollment or reinstatement for two years from the date of the denial (see 18 NYCRR §504.5(d)).
Searching the NY State Restrictions and Exclusions List
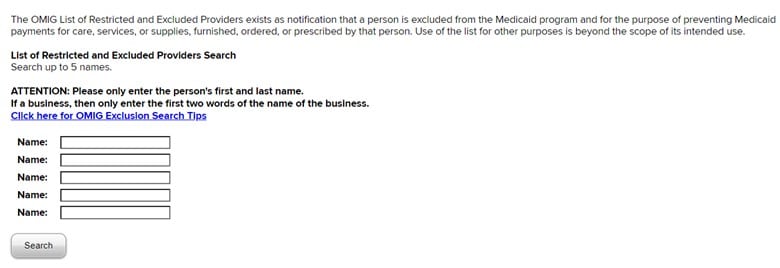
OMIG offers two options for searching the state’s Exclusions List which are similar to the processes available for searching the HHS-OIG’s List of Excluded Individuals/Entities (LEIE):
Web-based search function: A search can be conducted using the OMIG portal which allows up to five names to be searched at a time.
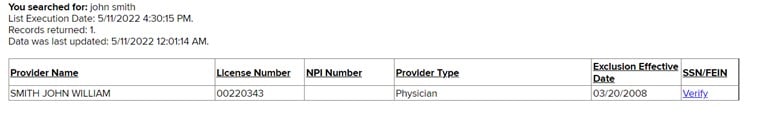
A search of “John Smith” using this search option produced the following:
There are also multiple downloadable options for access to the full state list:
- Formatted list – A complete, formatted copy of exclusions
- Tab delimited list – A complete list of exclusions suitable for importing into applications or desktop spreadsheets.
- Export to Excel – A complete list of exclusions for Excel.
- Short List – A list of exclusions that commenced in the last 30 days.
State Agencies Responsible for Management and Enforcement of Exclusion and Screening Requirements
OMIG
As noted above, OMIG is the primary state office responsible for management and enforcement of fraud, waste and abuse activities, including exclusion and sanctions, in New York. As of 2020, OMIG had 398 full-time equivalent staff working on Medicaid program integrity functions throughout the agency. These positions include auditors, investigators, nurses, data analysts, pharmacists, other clinical / medical professionals, program administrators/managers, and persons providing legal, technological, and clerical support.
The primary objectives of OMIG include the following:
- Promote, and advise upon Medicaid policies and procedures that advance or detract from program integrity objectives.
- Closely coordinate with New York State Department of Health (DOH) and other state agencies involved in the Medicaid program to identify their priorities and objectives and develop enforcement strategies that align with these priorities and objectives.
- Educate and collaborate with Medicaid providers and payers, including Managed Care Organizations (MCO), to improve their understanding and compliance with current Medicaid requirements and to tailor OMIG activities to minimize disruption.
- Monitor, identify and evaluate aberrant fiscal or programmatic trends and prioritize those that merit investigation or audit.
- Partner with and support other Federal, State, and local law enforcement and governmental agencies to identify inappropriate practices and enforce Medicaid rules and requirements.
- Cooperate, comment, and conduct appropriate follow-up actions, including the recovery of identified Medicaid overpayments, resulting from external audits of the NYS Medicaid program.
- Conduct audits in identified areas to assess provider compliance with Medicaid program and reimbursement practices to ensure that Medicaid recipients have access to quality medical services and that services are delivered efficiently. Where appropriate, OMIG publishes audit protocols in advance that are created in conjunction with the relevant state agencies and the provider community.
- Respond to allegations of fraud, waste, and abuse within the Medicaid program, initiate investigations of providers or recipients and take appropriate enforcement actions, including censure, exclusion, recipient restriction, or pre-payment review. OMIG also coordinates activities with the Special Investigation Units (SIU) of Medicaid managed care providers which strengthens program integrity and increases the numbers of referrals to OMIG.
- Referral of credible allegations or identified instances of fraud to the NYS Attorney General’s Medicaid Fraud and Control Unit (MFCU) for review, recovery, and potential prosecution. OMIG works closely with MFCU to identify and analyze trends while safeguarding that activities undertaken do not conflict with MFCU activities.
- Promote and provide opportunities for due process in the course of OMIG audits, investigations and reviews, and associated final agency actions
Medicaid Fraud Control Unit (MFCU)
As noted above, OMIG works closely with the New York Medicaid Fraud Control Unit (“MFCU” or “Unit”) which is headquartered in New York City and has seven regional offices: Albany, Buffalo, Hauppauge, New York City, Pearl River, Rochester, and Syracuse. The Unit is a division of the New York State Attorney General’s Office. The New York Unit is the largest of the 50 MFCUs across the nation.
The New York MFCU includes a Civil Enforcement Division which handles civil fraud investigations, including qui tam cases (whistleblower actions). The Unit also plays a significant role in the National Association of Medicaid Fraud Control Units’ (NAMFCU) global cases. Global cases are civil cases that involve both the Federal Government and a group of States.
The New York MFCU also includes an Electronic Investigative Support Group. This group organizes and analyzes State Medicaid claims data for MFCU investigations and manages the Unit’s computer network. Further, the Unit’s Electronic Investigative Support Group manages NAMFCU’s Global Case Repository. The repository is a centralized system that provides NAMFCU’s global case teams with the ability to coordinate their investigations and avoid duplication of efforts.
Referrals to the MFCU. The Unit receives referrals of fraud and patient abuse or neglect primarily from the State Medicaid agency, but also receives many referrals from private citizens and other State agencies. When the Unit receives a referral, the appropriate regional MFCU office determines whether to open a preliminary investigation, open a full investigation, or refer it to another agency.
Investigations. Once the Unit opens a preliminary or full investigation, regional managers assign a team to the case. Teams assigned to fraud cases generally include an investigator, attorney, auditor, and, as appropriate for the case, a nurse analyst. Cases of patient abuse or neglect are assigned a team consisting of an investigator, attorney, and a nurse analyst.
Prosecutions. The New York MFCU has Statewide criminal prosecutorial authority. If a case is not within the Unit’s prosecutorial authority, the MFCU typically refers it to either a district attorney or the appropriate United States Attorney’s Office. The Unit’s Civil Enforcement Division works jointly with Federal prosecutors on cases brought under the State False Claims Act.
New York Medicaid Contract Provisions Related to Exclusion and Screening:
The model New York Medicaid Managed Care contract with managed care organization includes the following sections and provisions related to exclusions and screening. The model contract, adopted for all 19 MCOs in New York State, requires MCOs, upon identifying “reasonably suspected” cases of fraud and abuse, to make referrals to the State Medicaid agency and OMIG. OMIG in turn refers such matters to the MFCU when it deems them to be credible allegations of fraud. Contractors are also subject to specific contractual requirements related to the identification and reporting of debarred or suspended individuals among its staff, vendors and contractors.
Section 18.05: FWA Reporting Requirements
(v) Pursuant to 42 CFR 438.608(a)(7), the Contractor shall refer all cases of potential fraud, waste, or abuse the Contractor identifies to SDOH and OMIG. Reporting of potential fraud, waste and abuse under this section includes all potential fraud, waste or abuse committed by, including but not limited to, the Contractor, Participating or Non-Participating Providers, subcontractors, vendors, Enrollees, rendering professionals, ordering or referring professionals, the Contractor’s or subcontractor’s employees, management or any third party
Section 18.10 Certification Regarding Individuals Who Have Been Excluded, Debarred or Suspended By Federal, State, or Local Government
- Contractor will certify to the SDOH initially and immediately upon changed circumstances from the last such certification that it does not knowingly have an individual who has been debarred or suspended by the federal, state or local government, or otherwise excluded from participating in procurement activities:
- as a director, officer, partner or person with beneficial ownership of more than five percent (5%) of the Contractor’s equity; or
- as a party to an employment, consulting or other agreement with the Contractor for the provision of items and services that are significant and material to the Contractor’s obligations in the Medicaid managed care program, consistent with requirements of SSA § 1932 (d)(1).
- Pursuant to 42 CFR 455. 436, the Contractor shall:
- confirm the identity and determine the exclusion status of any employee in the capacity of general manager, business manager, administrator, director, or other individual who exercises operational or managerial control over, or who directly or indirectly conducts the day-to-day operations at initial hiring and any person with an ownership or control interest or who is an agent or managing employee of the Contractor through routine checks of Federal and State databases. These include the Social Security Administration’s Death Master file (SSDM), the National Plan and Provider Enumeration System (NPPES), the Excluded Parties List System or the System for Award Management (EPLS/SAM), and either the List of Excluded Individuals and Entities (LEIE), the NYS OMIG Exclusion List, the United States Department of the Treasury’s Office of Foreign Assets Control Sanctions List and any such other databases as the Secretary may prescribe; and
- check the LEIE, the EPLS/SAM and NYS OMIG Exclusions List and the United States Department of the Treasury’s Office of Foreign Assets Control Sanctions List no less frequently than monthly.
- Pursuant to 42 CFR 455.436 and 42 CFR 438.610, the Contractor shall:
- confirm the identity and determine the exclusion status of new Participating Providers, re-enrolled Participating Providers and all current Participating Providers, any subcontractors, and any person with an ownership or control interest or who is an agent or managing employee of the Participating Provider or subcontractor through routine checks of Federal and State databases. These include the Social Security Administration’s Death Master file (SSDM), the National Plan and Provider Enumeration System (NPPES), the Excluded Parties List System or the System for Award Management (EPLS/SAM), the List of Excluded Individuals and Entities (LEIE), the NYS OMIG Exclusion List, the United States Department of the Treasury’s Office of Foreign Assets Control Sanctions List, and any such other databases as the Secretary may prescribe; and
- confirm the identity and determine the exclusion status of Non-Participating Providers, upon or no later than 30 days of payment of first claim through routine checks of Federal and State databases. These include the Social Security Administration’s Death Master file (SSDM), the National Plan and Provider Enumeration System (NPPES), the Excluded Parties List System or the System for Award Management (EPLS/SAM), the List of Excluded Individuals and Entities (LEIE), the NYS OMIG Exclusion List, the United States Department of the Treasury’s Office of Foreign Assets Control Sanctions List and any such other databases as the Secretary may prescribe; and
- check the SSDM and NPPES for new providers, re-enrolled providers and any current provider who were not checked upon enrollment into Contractor’s Medicaid program; and
- check the LEIE, the EPLS/SAM, and the NYS OMIG Exclusion List no less frequently than monthly.
- The Contractor must:
- confirm that providers have procedures in place to identify and determine the exclusion status of managing employees through routine checks of Federal databases. These include the Social Security Administration’s Death Master file, the National Plan and Provider Enumeration System (NPPES), the Excluded Parties List System (EPLS), either the List of Excluded Individuals and Entities or the Medicare Excluded Database (MED), and any such other databases as the Secretary may prescribe; and
- check the LEIE (or the MED), the EPLS and the NYS OMIG Exclusion List no less frequently than monthly.
Section 18.13 Disclosure of Criminal Activity
- Pursuant to 42 CFR 455.106, the Contractor will disclose to SDOH any criminal convictions by managing employees related to Medicare, Medicaid, or Title XX programs at the time the Contractor applies or renews an application for participation in the Medicaid managed care program or at any time on request. For the purposes of this section, managing employee means a general manager, business manager, administrator, director, or other individual who exercises control or who directly or indirectly conducts the day-to-day operation of an institution, organization, or agency.
- Pursuant to 42 CFR 455.106, before the Contractor enters into or renews a provider agreement, or at any time upon written request by the State, the Contractor must disclose to the State the identity of any person who:
- has ownership or control interest in the provider, or is an agent or managing employee of the provider; and
- has been convicted of a criminal offense related to that person’s involvement in any program under Medicare, Medicaid, or the Title XX services program since the inception of those programs.
- Notification to the U.S. Department of Health and Human Services (DHHS) Inspector General.
- The SDOH shall notify the DHHS Inspector General of any disclosures made this section within 20 working days from the date it receives the information; and
- The SDOH must also promptly notify the DHHS Inspector General of any action it takes with respect to the provider’s participation in the program.
- Denial or Termination of Provider Participation
- The Contractor shall refuse to enter into or renew an agreement with a provider if any person who has an ownership or control interest in the provider, or who is an agent or managing employee of the provider, has been convicted of a criminal offense related to that person’s involvement in any program established under Medicare, Medicaid or Title XX services program; and
- Unless authorized by the SDOH, the Contractor may refuse to enter into or may terminate a provider agreement if it determines that the provider did not fully and accurately make any disclosure required under Section 18.12(b).
- Such denial or termination of a provider’s participation under this section may afford the provider a right to a hearing pursuant to Public Health Law § 4406-d (2).
Section 21.2 Medicaid Advantage Network Requirements
(b) The Contractor shall not include in its network any provider:
- who has been sanctioned or prohibited from participation in federal health care programs under either Section 1128 or Section 1128A of the SSA; or
- who has had his/her license suspended by the New York State Education Department or the SDOH Office of Professional Medical Conduct.
Section 21.3 SDOH Exclusion or Termination of Providers
- If SDOH excludes or terminates a provider from its Medicaid Program, the Contractor shall, upon learning of such exclusion or termination, immediately terminate the Provider Agreement with the Participating Provider with respect to the Contractor’s Medicaid Advantage Product, and agrees to no longer utilize the services of the subject provider, as applicable. The Contractor shall access information pertaining to excluded Medicaid providers through the SDOH Health Commerce System (HCS). Such information available to the Contractor on the HCS shall be deemed to constitute constructive notice. The HCS should not be the sole basis for identifying current exclusions or termination of previously approved providers. Should the Contractor become aware, through the HCS or any other source, of an SDOH exclusion or termination, the Contractor shall validate this information with the Office of Health Insurance Programs and comply with the provisions of this Section.
- Consistent with 42 CFR 455.416(c), if a Participating Provider has been terminated, as defined in 42 CFR 455.101, on or after January 1, 2011, under the Medicare program, the Medicaid program or CHIP program of any other State, or the network of another NYS Medicaid Managed Care Organization, the Contractor shall, upon notification of such termination from SDOH or OMIG, immediately terminate the Provider Agreement with the Participating Provider with respect to the Contractor’s Medical Advantage Product, and agrees to no longer utilize the services of the subject provider, as applicable.
- If Medicaid payments are made by the Contractor to an excluded or terminated provider for dates of service after the provider’s exclusion or termination effective date, the Contractor shall report and explain within 60 days of identifying the overpayment, in a form and format to be determined by OMIG in consultation with SDOH, when and how the overpayment was identified, and the date on which the encounter data was adjusted to reflect the recovery.































