In June, 2022, the OIG issued its 2021 Iowa Medicaid Fraud Unit (MFCU) Inspection Report. The OIG inspection revealed a MFCU unit with exceptionally strong case outcomes over the 2019-2021 period compared to other similarly-sized state units. For the federal fiscal years (FYs) 2019– 2021, the work of the Iowa MFCU resulted in 80 indictments, 79 convictions, 36 civil settlements/judgments and $9.2 million in recoveries.
These statistics reflect the positive collaboration between the MFCU and county prosecutors because the MFCU does not have prosecutorial authority and most commonly refers cases for prosecution to Iowa’s 99 county attorneys’ offices. It is the opinion of the OIG that the Unit’s ability to refer cases for prosecution to the county attorneys is a significant prosecutorial resource for the Unit and allows cases to be fully adjudicated with limited delays. Further, the Unit reported that investigators had strong relationships with many of the county attorneys, and that cases were rarely declined for prosecution. Additionally, through the OIG review of case files and interviews with multiple stakeholders, the OIG made the observation that the Unit performed thorough investigations and provided complete and well-organized investigative reports, which likely contributed to swift and positive case resolutions. Finally, the ability to refer cases for external prosecution allowed the Unit to focus its efforts on investigations, and the OIG found that the Unit maintained a continuous case flow by implementing a number of practices that improved efficiency and timeliness
Findings & Observations
The OIG found that the Iowa Unit generally operated in accordance with applicable laws, regulations, and policy transmittals and the MFCU performance standards. The findings and observations were minimal and those commonly found in the OIG’s MFCU inspection reports in other jurisdictions:
- Finding: Staffing Levels. The Unit did not maintain staffing levels in accordance with its approved budget, maintained low staffing levels in relation to State Medicaid expenditures, and experienced significant turnover of investigators and high caseloads.
While the total number of investigators employed remained consistent during the review period (four investigators at the end of each fiscal year) there was significant turnover of investigators. During this period, the Unit hired five new investigators and six investigators left. Of the six investigators who left, four were employed with the Unit for short periods—between 1 week and 15 months. Two of the six investigators who left the Unit did not complete the Unit’s 6-month probationary period and the other four left due to general attrition, such as retiring or taking another job. Three long-time investigators remained employed with the Unit throughout the review period. Another reason for the low staffing levels was the Unit’s strategic response to the COVID-19 pandemic. Specifically, the Unit reported that it strategically did not fill investigator vacancies during the pandemic because of the reduced number of referrals it received and because of pandemic-related limitations on the Unit’s ability to investigate patient abuse or neglect.
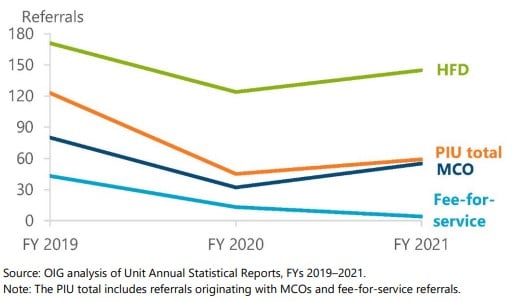
The OIG recommended that the state assess the adequacy of existing staffing levels, and if warranted, develop a plan to expand the size of the Unit. The OIG also recommended that the state should consider what caused the investigator turnover and what actions might mitigate that factor. - Observation: Reduced Referrals. The Unit took steps to maintain an adequate volume and quality of referrals, but referrals from key sources generally decreased during the review period. During the review period, the Unit received 227 fraud referrals from the state’s Program Integrity Unit (PIU) which is responsible for Medicaid fraud oversight; 60 of these were from the fee-for-service component of the Medicaid program and 167 originated with managed care organizations (MCOs) which provider coverage for the majority of Iowa’s Medicaid population. During this period, fee-for-service referrals from the PIU declined dramatically, and referrals from the PIU that originated with MCOs decreased in FY 2020 and increased modestly in FY 2021.
Several factors contributed to this decline:
- In 2020 the PIU modified its long-standing practice of referring all cases of potential fraud to the Unit and began to only refer cases for which documentation supported a “credible allegation of fraud.”
- MCOs changes in the Iowa Medicaid program. These transitions disrupted MCO program integrity operations, limiting the number and quality of referrals to the Unit for a period of time following the changes.
- The COVID-19 pandemic resulted in significant decreases in referrals relate to patient abuse/neglect. Long-term care complaints to HFD decreased in FY 2020 because of limits on the state’s survey activity and restricted visitation in long-term care facilities, which in turn limited the number of complaints referred to the MFCU.
On a very positive note, the OIG included several observations which reflect the successes of the Unit:
- Regarding the performance standard related to “Cooperation with Federal Authorities on Fraud Cases, the OIG made the following observations:
- The Unit maintained a positive working relationship with Federal law enforcement partners, including OIG and U.S. Attorney’s Offices. During the review period, the Unit reported working 38 joint cases with OIG’s Office of Investigations (OI). The Unit director communicated regularly with OI management, and Unit investigators maintained strong working relationships with OI agents. The Unit also maintained positive working relationships with both U.S. Attorney’s Offices in Iowa.
- The Unit submitted all convictions and adverse actions to Federal partners within the appropriate timeframes. During the review period, the Unit submitted all of its 84 convictions to OIG within 30 days of sentencing, as required by Performance Standard 8(f). The Unit also submitted all of its 84 adverse actions to the NPDB within 30 days of the final adverse action, as required by Federal regulations. The failure to timely report is a common finding in OIG Unit inspection reports. That the Iowa MFCU, notwithstanding the noted staffing challenges, met these deadlines is even more noteworthy.
- Observation: The Unit took steps to maintain a continuous case flow and to complete cases within appropriate timeframes. MFCU supervisors are required to approve the opening and closing of all investigations, review the progress of cases, and take action as necessary to ensure that each stage of an investigation is completed within an appropriate timeframe. The OIG review reflected adherence to these requirements. Further, nearly all case files contained appropriate documentation of supervisory approval for case openings and applicable case closings, as well as applicable quarterly reviews of case files.
Several best practices may have contributed to this case flow:- First, case assignments were made to investigators on the basis of their preferences and expertise. Unit staff and management identified this practice as highly beneficial to productivity and timeliness of cases. One staff member stated that, because of the investigators’ areas of expertise, when the investigators “go out to investigate, they’re well-versed and know what to look for and what to ask. They know how to interpret the evidence they get back.”
- Another practice that contributed to continuous case flow was that the director developed a case plan, which he shared with the investigator when assigning the case. The case plan established the scope of the investigation and the primary allegations to be investigated; determined any necessary coordination with law enforcement partners; and addressed any additional administrative, procedural, or investigative issues. The case plan established a date by which the investigator was expected to submit a case to be closed or to be reviewed for referral for prosecution. The investigation completion date was flexible and could be modified as needed as the investigation progressed. The timelines for investigations were also incorporated into the investigators’ performance evaluations, which the director believed provided incentive to complete cases in a timely manner.
- Finally, to improve investigators’ efficiency, the Unit transferred responsibility for administrative duties from the investigators to the Unit’s paralegal. The director’s goal in doing so was to have investigators focusing solely on investigative activities. For example, investigators did not have to track their cases after they were referred and accepted for prosecution. Those cases were transferred to the Unit’s paralegal for monitoring.
Conclusion
The Iowa Unit concurred with the OIG’s recommendation to assess the adequacy of existing staffing levels, and if warranted, develop a plan to expand the size of the Unit. In its response, the Unit indicated that it had hired an additional investigator in the period following the OIG onsite inspection. The Unit stated, on the basis of its most recent staffing assessments, that its current staffing level is sufficient to respond to its current volume of referrals and to ensure reasonable investigative caseloads. The Unit noted that as it continues to develop and enhance referral sources in order to increase the number of investigations, it will continue to assess existing staffing levels and fill vacant investigator positions when appropriate to do so.


































