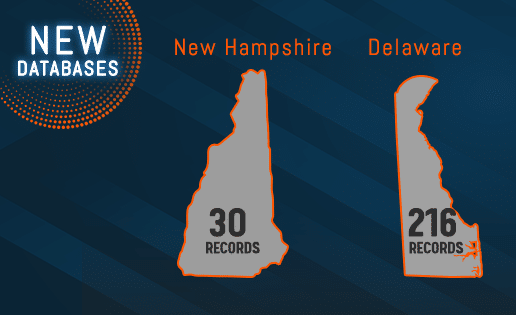
Healthcare organizations are now able to screen against the state exclusion databases of both New Hampshire and Delaware. They are the latest addition to Streamline Verify’s database portfolio. This brings the total to 44 states which carry lists of excluded individuals and entities in their respective territories.
New Hampshire
The Program Integrity Unit (PI) spearheads the Medicaid concerns of the New Hampshire Department of Health and Human Services (HHS-NH). It examines financial claims for possible cases of fraud, waste or abuse. Instances of actual or potential fraudulent activity is elevated to the Attorney General’s Office for further investigation. Furthermore, the PI determines the appropriateness of medications used as well as checks the quality and need for hospital admissions.
Medical providers and professionals found to be unqualified to participate on valid grounds are terminated from its Medicaid program. They are placed under the New Hampshire Medicaid Provider Exclusion and Sanction List along with the basis for doing so. It updates monthly and disqualified participants dating from April 1, 2013 can be viewed. Checking the HHS-OIG Exclusion, the System for Award Management and other exclusions databases however is still firmly required.
The HHS-NH also employs the use of a Fingerprint-based Criminal Background Check (FCBC) system. It further precludes the chances of violators participating in its Medicaid program. This is based on Section 6401 of the Affordable Care Act. Those having five percent ownership whether directly or indirectly and are considered as “high risk” pursuant to 42 CFR 455.450 have additional requirements. They must be subjected to a national and state criminal background check as well as an FCBC.
Delaware
The Delaware Health and Social Services likewise tracks instances of fraud, waste and abuse within its State Medicaid program. It accomplishes this through its Division of Medicaid and Medical Assistance Program Integrity Unit. Compliance is reinforced by its PI through the following instances:
- Audits
- Education
- Prevention
- Recovery of improper payments
- Third party liability
Residents can also assist the PI unit by privately reporting Medicaid fraud violators through its hotline. While Delaware does have an exclusion database, it is not presently available to the general public online.
Those employing or transacting with excluded individuals and entities on its list could potentially be liable for Civil Monetary Penalties. Remember that the HHS-OIG’s own federal exclusion database might not carry all the excluded names on a per state level.
Comprehensive Coverage
Streamline Verify’s technology gives businesses the ability to cover a wide range of databases. This supports a more thorough check for excluded individuals and entities. Clients are not limited to just the State or federal level sanction lists. There are also licensing lists and other important sanction lists that are available for screening to ensure complete compliance.
Please refer to this resource for more helpful information on OIG Exclusion Screening.


































